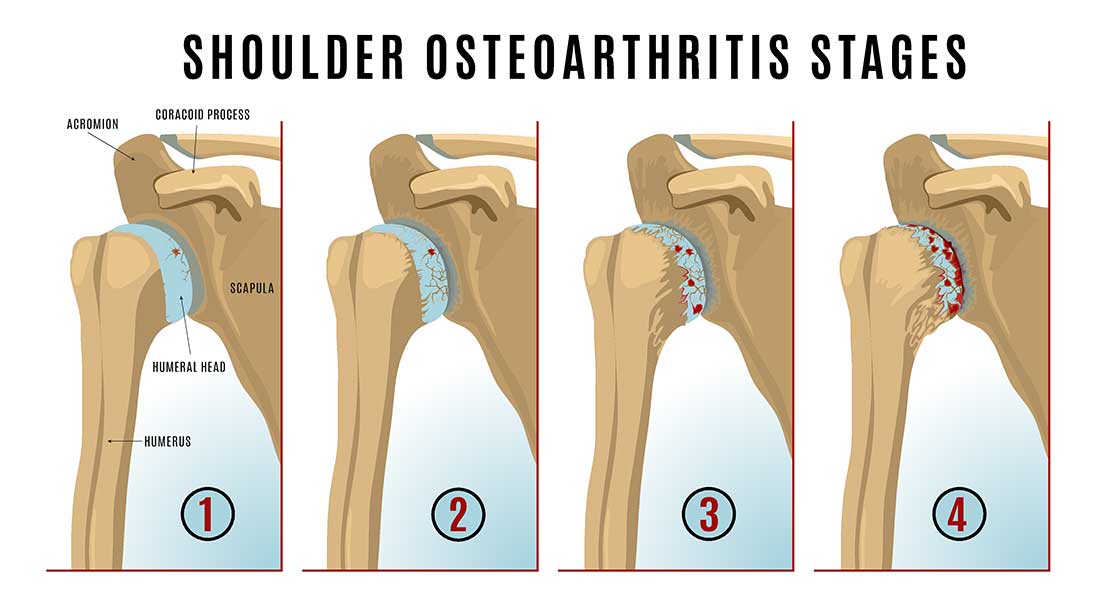
The shoulder, like any other joint, can be affected by wear and tear over years of use. With time, the hard, shiny surfaces of the joint (the articular cartilage), may begin to roughen and break down. This is known as osteoarthritis. As it progresses, the joint surfaces no longer slide smoothly over each other but start to grate and grind, and the cartilage continues to break down until eventually there is bare bone grinding on bare bone. This can be incredibly painful and cause stiffness and loss of strength.
Two main areas of the shoulder tend to be affected by osteoarthritis – the ball and socket part of the shoulder (‘glenohumeral’ joint) and the smaller joint on top of the shoulder (acromioclavicular joint)

If you have shoulder arthritis, you may experience pain, particularly when moving the shoulder, or whilst trying to sleep at night.
Your shoulder may feel stiff first thing in the morning, and you may notice that your range of movement is limited: you might find it difficult to comb your hair, for example, or put on a shirt, and there may be clicking or grinding sounds and odd sensations when moving your shoulder.
Some patients will also experience neck pain, or pain in their upper back, because the shoulder isn’t moving correctly.
When we meet, I’ll ask you lots of questions about how your shoulder is affecting you, I’ll examine your shoulder and look at how you move and how your muscles are functioning.
In the majority of cases, I will arrange a scan of your shoulder, which may be an X-ray or MRI, to see how badly the cartilage is worn, and also to see if there is any other damage to the supporting structures and muscles around the joint, such as the rotator cuff.
Treatment options will depend on what symptoms are causing you the most problems. If it is pain, then we can work together to relieve this, possibly with steroid injections and/ or increased oral painkillers. Weakness, stiffness and reduced range of movement can be addressed with physical therapies such as physiotherapy or osteopathy. Often, we use a combination of injections, painkillers and physical therapy to relieve the early symptoms of arthritis.
Unfortunately, arthritis tends to be progressive, and your symptoms may gradually return, or worsen, despite these initial measures. Should this happen then we should start to think about shoulder surgery.
If your shoulder joint is very worn, and you are struggling with pain, stiffness or loss of function, it may be necessary to replace the whole joint, or parts of the joint.
In this situation, I will arrange further imaging of your shoulder, usually a CT and/ or MRI scan, to give me a good idea of what is going on in the joint, and help me to plan the operation in advance.
A shoulder replacement is a big undertaking, but it can be extremely helpful in terms of reducing pain, and increasing function, for the majority of patients. Around 85-90% of patients will have a good outcome and, in most cases, the replacement lasts a long time – around 15 years.
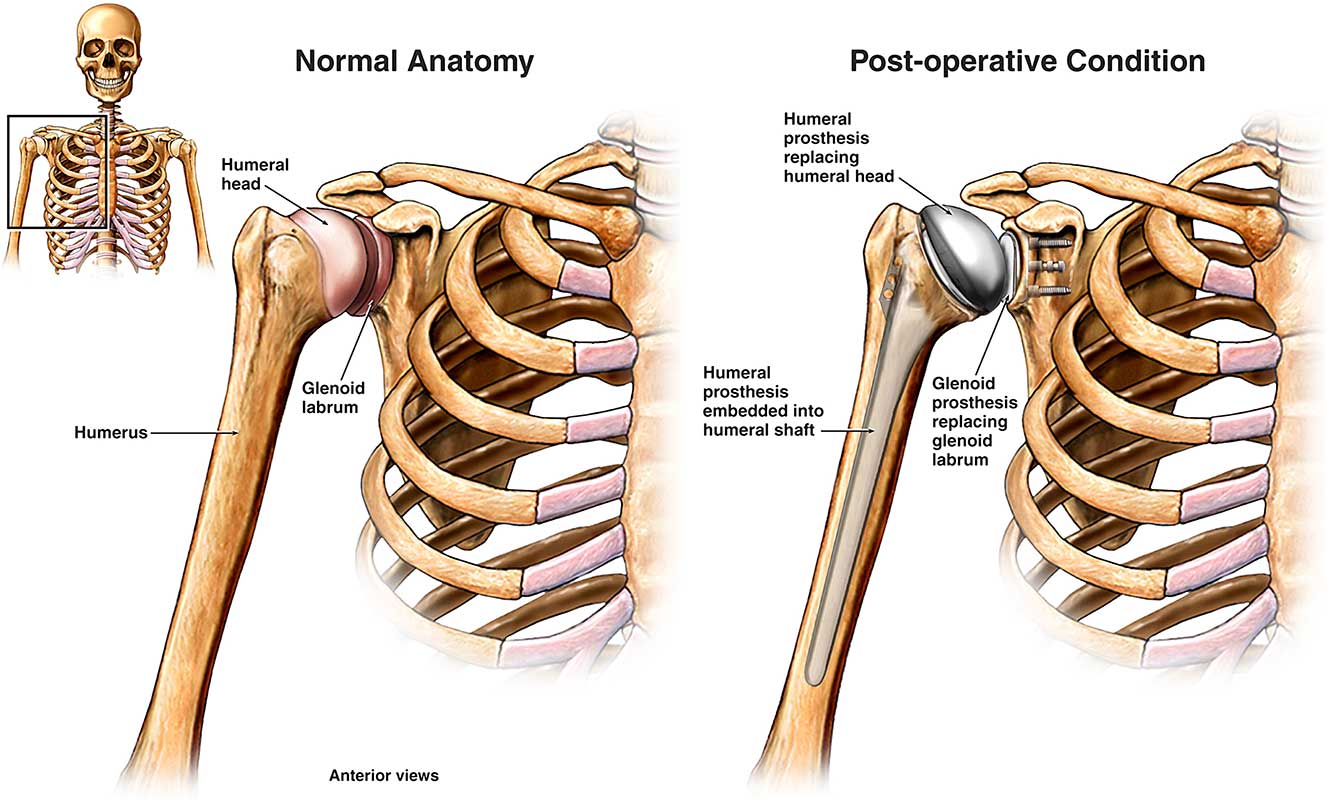
During a shoulder replacement operation, the damaged surfaces of the shoulder are removed, and replaced with new components.
Sometimes only one side of the shoulder needs to be replaced, and this known as a ‘hemi arthroplasty’.
This type of surgery is less common, because osteoarthritis typically affects both sides of the joint, and usually, a total shoulder replacement (‘total shoulder arthroplasty’) is the best option.
A total shoulder arthroplasty is suitable for people who have a worn joint, but whose supporting tissues, such as the rotator cuff muscles, ligaments and tendons, are still intact and are able to hold the shoulder in place.
The wear and tear which has caused your shoulder osteoarthritis can also damage the other structures in the shoulder, in particular the rotator cuff muscles or tendons
If these are significantly torn, then a more complicated ‘Reverse Geometry’ shoulder replacement may be required (see below).
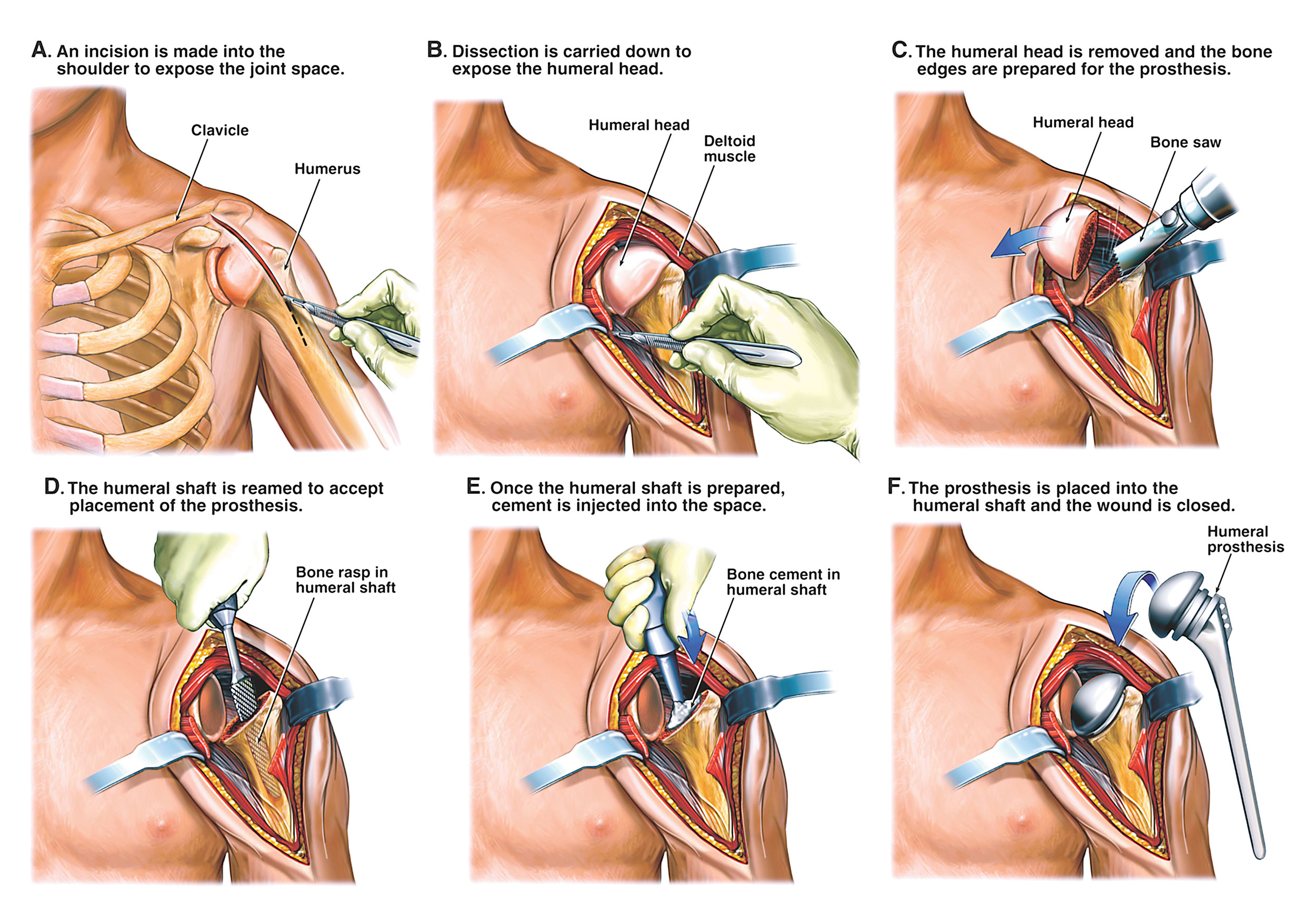
Shoulder replacement surgery takes place under a general anaesthetic (so you’ll be asleep), and to help with pain after the surgery, we’ll perform some nerve blocks to numb the shoulder. Most patients go home the day after the surgery.
It’s not possible to perform shoulder replacement with keyhole surgery and so an incision is made along the contour of the shoulder. One of the tendons is cut to get access to the ball and socket joint, and this is repaired after the two sides of the joint have been replaced.
After the operation, it’s very important that sufficient recovery time be given in order for the tendon to heal and to recover, and also for the replaced surfaces to knit with the bones of the shoulder.
Whilst you’re in hospital, you’ll be seen by a physiotherapist who will guide you through some gentle exercises in the form of pendulum movements of the arm. Over time you’ll progress through moving the shoulder through a bigger range of movement, and exercises to strengthen the shoulder.
Below is a diagram showing the steps in a partial shoulder replacement. For a total shoulder replacement there is also a component attached to the shoulder blade, as shown in the sections above and below
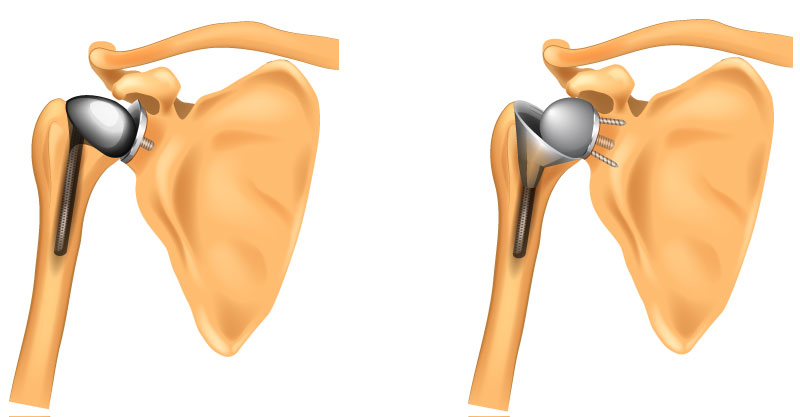
If you have a very worn shoulder, and the rotator cuff tendons that support the stability of the shoulder have torn through wear and tear, then I might advise that you have a reverse geometry replacement. This is when the shoulder is replaced with a new ball and a new socket that are placed the opposite way around. This configuration means that you can move your shoulder using the deltoid muscle alone and you don’t have to rely on the rotator cuff tendons being intact.
Below is a picture of a total shoulder replacement on the left and a reverse shoulder replacement on the right.
No surgery is without risk, but thankfully the risks are low for shoulder replacement surgery. There is a risk of infection (around 1-2 %), fracture of the bones, dislocation of the shoulder, bleeding and nerve damage, but the majority of patients will have an outcome that they are happy with.
Shoulder replacements are made up of mechanical components that are not natural, and eventually, they will fail at some point. What tends to happen is that the components loosen within the joint, and the shoulder begins to become painful again.
It doesn’t often happen before 15 years, but occasionally some early loosening does occur.
Good rehab in the form of physiotherapy or osteopathy will enable you to get the best out of your surgery, but It will take some time and several months before you really feel the true benefits.
Shoulder replacement surgery can be a really good solution for you if you have severe shoulder arthritis symptoms.
